Safe walking timeline, benefits, and tips for C-section recovery. Expert guidance for new moms on postpartum mobility and healing.
Bringing your baby into the world via cesarean section is major abdominal surgery, and your body needs time to heal. But here’s something that might surprise you: gentle walking after C – Section is actually one of the best things you can do for your C-section recovery. Let’s talk about how to safely get moving again and why it matters so much for your healing journey.
Why Walking Matters After a C-Section

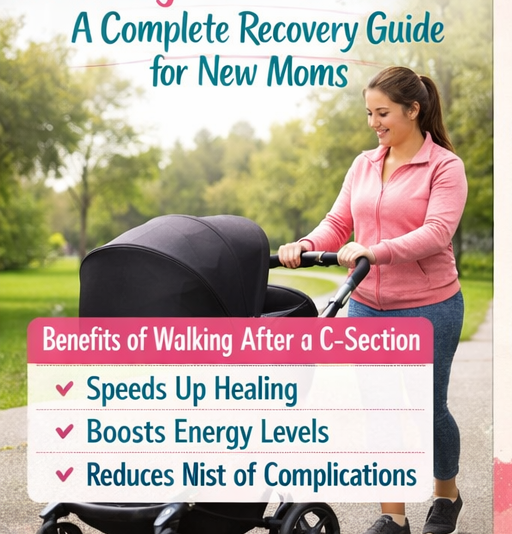
Walking after your cesarean delivery isn’t just about getting back to normal life. It serves several critical purposes in your recovery. Movement helps prevent blood clots, which is one of the most serious complications after any surgery. When you walk, even just a little bit, you improve circulation throughout your body and reduce the risk of deep vein thrombosis.
Walking also helps your digestive system wake up after surgery. Many C-section moms experience gas pain and bloating in the days following delivery, and gentle movement can ease these uncomfortable symptoms by getting your bowels moving again. Additionally, walking reduces your risk of developing pneumonia by encouraging you to breathe more deeply and expand your lungs fully.
When Can You Start Walking After a C-Section?
The timeline for walking varies depending on your individual recovery, but here’s what most new moms can expect. Within 12 to 24 hours after your surgery, your medical team will encourage you to take your first steps. Yes, this sounds incredibly soon, and yes, it will feel difficult. Those first steps might just be from your bed to a chair or to the bathroom, and that’s perfectly fine.
Your nurse will typically help you with this first walk. You’ll move slowly, supporting your incision with your hands or a pillow, and you might feel dizzy or lightheaded. This is normal. The goal isn’t distance or speed but simply getting your body upright and moving. During your hospital stay over the next two to four days, you’ll gradually increase how often and how far you walk, always within your comfort level.
Week-by-Week Walking Guidelines
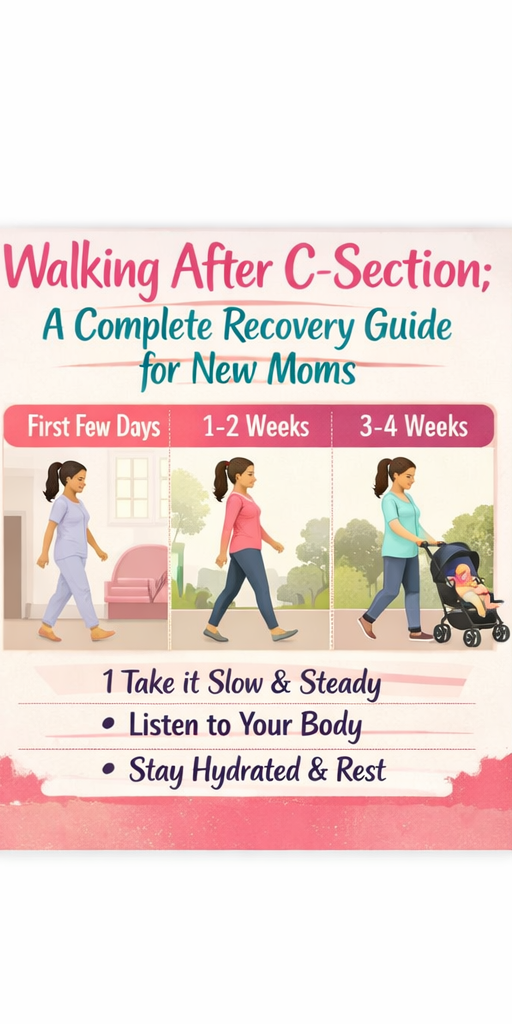
Week One: During your first week at home, focus on short, frequent walks around your house. Five to ten minutes several times a day is ideal. Your incision will still be quite tender, and you’ll tire easily. Listen to your body and rest when you need to. Don’t push through significant pain.
Weeks Two to Four: As you move through your second and third weeks, you can gradually increase your walking duration. Aim for 15 to 20-minute walks once or twice daily. You might feel ready to venture outside for short walks around your neighborhood. Pay attention to how your body responds and don’t increase your activity too quickly.
Weeks Four to Six: By your fourth week, many moms feel considerably better and can walk for 20 to 30 minutes at a time. However, remember that you’re still healing internally, even if your incision looks good externally. Your six-week postpartum checkup is when your doctor will clear you for more intensive exercise, but walking remains an excellent choice during this period.
Important Warning Signs to Watch For
Stop walking immediately and contact your healthcare provider if you experience any of these symptoms: increased bleeding or bright red blood, sudden sharp pain at your incision site, fever over 100.4°F, increased swelling or redness around your incision, dizziness or feeling faint, or separation of your incision edges. These could indicate complications that need medical attention.
Tips for Safe and Comfortable Walking
Start each walking session by supporting your incision with your hands, a small pillow, or an abdominal binder if your doctor has recommended one. This support reduces pulling sensations and provides comfort as you move. Wear comfortable, supportive shoes, even for short walks around your home. Your center of gravity has shifted during pregnancy, and proper footwear helps prevent falls.
Good posture makes a significant difference in your comfort level. Stand tall with your shoulders back, even though you might feel like hunching over to protect your incision. Slouching actually creates more tension and discomfort. Walk on flat, even surfaces initially to minimize the risk of tripping or jarring your healing abdomen.
Stay hydrated before, during, and after your walks. Your body is working hard to heal, and if you’re breastfeeding, you need even more fluids. Bring water with you or plan your route past places where you can get a drink.
What to Avoid in the First Six Weeks
While walking is encouraged, certain activities need to wait until your doctor clears you. Avoid any high-impact exercise like running, jumping, or aerobics classes. Don’t lift anything heavier than your baby, which means no carrying toddlers, laundry baskets, or groceries. Skip exercises that engage your core muscles directly, such as sit-ups, crunches, or planks. These can stress your healing abdominal muscles and incision.
Don’t walk through significant pain. Some discomfort is normal, but sharp or severe pain is your body’s signal to stop. Avoid stairs as much as possible in the first week, and when you must use them, take them slowly one step at a time.
Making Walking Work with a Newborn

Finding time to walk with a brand-new baby can feel impossible, but small strategies help. If your baby likes the stroller or carrier, take them with you on short walks. The motion often soothes fussy babies, and you both benefit from fresh air. However, wait until your doctor clears you for wearing your baby in a carrier, as this adds weight and changes your center of gravity.
Ask your partner or a family member to watch the baby while you take a quick walk. Even 10 minutes alone can provide physical and mental health benefits. Some moms find that walking while their baby naps works well, though you should never feel guilty about resting during those precious sleep windows instead.
Consider walking with other new moms. Many communities have postpartum walking groups specifically for women recovering from childbirth. The social connection and mutual support can be just as valuable as the physical activity.
Mental Health Benefits of Walking
The physical benefits of walking after a C-section are clear, but the mental health advantages deserve equal attention. Gentle exercise releases endorphins, which improve your mood naturally. Getting outside exposes you to sunlight, which helps regulate your sleep-wake cycle and can reduce symptoms of postpartum depression and anxiety.
Walking provides a break from the intensity of newborn care. Those minutes of movement give you time to process your birth experience, adjust to motherhood, and simply exist as yourself rather than solely as a caregiver. Many new moms find that walking helps clear their mind and reduce the feeling of being overwhelmed.
Gradually Returning to Exercise
Walking serves as the foundation for eventually returning to your regular exercise routine. Once your doctor clears you at your six-week appointment (or later if you had complications), you can slowly add other activities back into your life. Continue walking while gradually introducing gentle stretching, pelvic floor exercises, and eventually strength training.
Some moms benefit from working with a physical therapist who specializes in postpartum recovery. They can assess your core and pelvic floor function, identify any diastasis recti (abdominal separation), and create a personalized exercise plan that supports safe recovery.
The Bottom Line
Walking after a C-section is both safe and beneficial when done properly. Start slowly, listen to your body, and gradually increase your activity level as you heal. Every mom’s recovery is different, so don’t compare your progress to others. What matters is that you’re taking care of yourself and giving your body the movement it needs to heal well.
Remember that you’ve just undergone major surgery while also beginning the demanding work of caring for a newborn. Be patient with yourself. Some days you’ll feel strong and capable, other days you’ll need more rest. Both are normal parts of recovery. Walking is a tool to support your healing, not another task to stress about or feel guilty for not doing perfectly.
Your body has done something incredible by bringing your baby into the world. Treat it with kindness, respect its signals, and celebrate each small step forward in your recovery journey.
Check out my another C section topics : What to Eat after C- Section: My Story